The Bladder Cancer Challenge
High unmet needs for detection, diagnosis and management in the early, non-muscle-invasive stages of bladder cancer.1–3
Bladder cancer is a major challenge around the world.4 Improving the way this disease is detected, diagnosed and managed can save lives.2,5 Equally important, it can improve patients' quality of life, while helping health systems and payers to reduce costs and provide care to more people.2,6
What is bladder cancer? What is NMIBC?
Bladder cancer is the growth of a tumor (abnormal cells) in the bladder that is classified into two types, depending on the depth of invasion in the bladder wall:7,8
- Non-muscle invasive bladder cancer (NMIBC) is restricted to the inner layer of cells that line the bladder and accounts for ~75% of all bladder cancer cases.3,7,8
- Muscle-invasive bladder cancer (MIBC) refers to the stage where the cancer has grown into the muscle layers of the bladder wall.7,8 This type is more likely to spread7,8
If bladder cancer has spread beyond the bladder itself, it is referred to as advanced or metastatic bladder cancer.7 The likely outcome of having bladder cancer—the bladder cancer prognosis—varies with the type of bladder cancer.
A frequently occurring cancer
Bladder cancer is a huge challenge globally. Bladder cancer ranks as the 8th most common cancer worldwide – the 5th most common in men – with 1 949 000 prevalent cases (5-year prevalence rate)4a, 614 000 new cases and more than 220 000 deaths in 2022.4b
Bladder cancer affects men more frequently than women, with incidence and mortality rates three times those in women.4 The disease occurs mainly in older people: approximately 90% of people with bladder cancer are older than 55.9
The management of bladder cancer and the patient journey
Patients must navigate a long process of diagnosis, treatment and follow-up.1 As bladder cancer has a relatively high risk of recurrence and progression (i.e. there is a high bladder cancer recurrence rate),1,2 the patient can expect regular surveillance and potential re-treatment.1
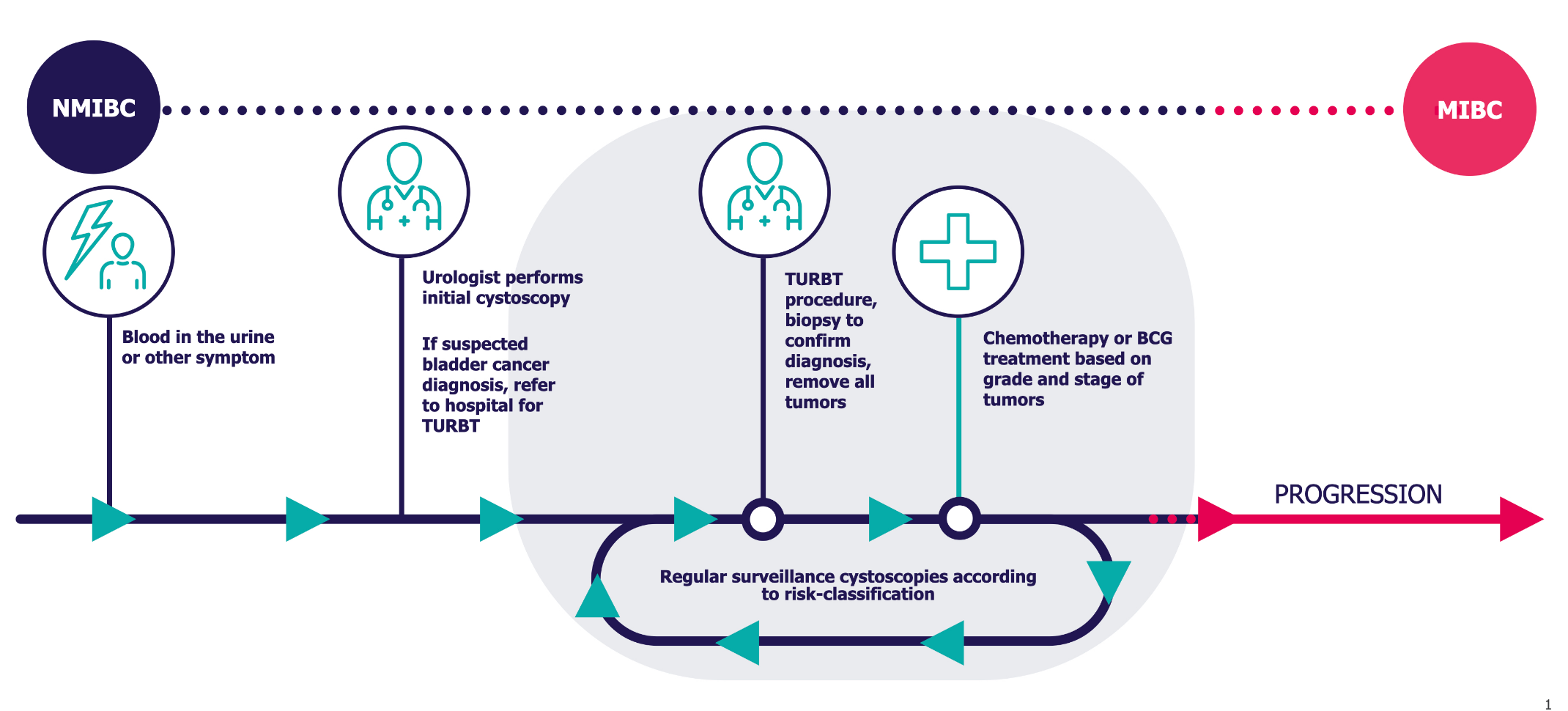
A cystoscopy or cystoscopy procedure is the use of an instrument called a cystoscope (a thin camera) to examine the inside of the bladder. For the initial assessment of the bladder as well as later controls, a flexible cystoscopy with a thin, bendy cystoscope would normally be used. For surgical procedures which are commonly performed under general anesthesia, a rigid cystoscopy with a slightly wider cystoscope that does not bend would be used. Cystoscopy for men and women is carried out in the same way.10
Different types of cystoscopic equipment exists and different types of light can be used for visualization of cancer. The Photocure technology utilizes blue light cystoscopy for cancer visualization.11,12
Expensive to manage
Bladder cancer is a costly, potentially progressive disease for which patients have to undergo multiple cystoscopies due to the high risk of recurrence.2
The paper, "Economic Burden of Bladder Cancer Across the European Union" estimates that bladder cancer cost the EU €4.9 billion in 2012.13 The estimated total cost to treat newly diagnosed and newly recurrent patients in the U.S. in 2021 exceeds $6.5 billion.14
The scale of this cost underlines the need to improve both the diagnosis and the management of bladder cancer for the benefit of patients, healthcare systems and payers.1,2,13,14
An opportunity to
transform bladder
cancer management
Better control of bladder cancer to address the bladder cancer survival rate can save lives, improve the quality of life of patients and reduce the cost of managing it.2,5,6
Photocure is dedicated to leading change in bladder cancer.
References
1. Babjuk M et al. Eur Urol 2019; 76(5): 639–657.
2. Witjes JA et al. Eur Urol 2014; 66(5): 863–871.
3. Cheung G et al. BMC Med 2013; 11: 13.
4. Globocan. a) 5-year prevalence / b) incidence/mortality by population. Available at: https://gco.iarc.fr/today. Accessed February 2024.
5. Chamie K et al. Cancer 2013; 119(17): 3219–3227.
6. Mogensen K et al. Scand J Urol 2016; 50(3): 170–174.
7. NHS. Bladder Cancer. 2018. Available from: https://www.nhs.uk/conditions/bladder-cancer. Accessed September 2021.
8. American Cancer Society. About Bladder Cancer. 2021. Available from: https://www.cancer.org/cancer/bladder-cancer/about.html. Accessed September 2021.
9. Cancer.net. Bladder Cancer: Statistics. 2021. Available from: https://www.cancer.net/cancer-types/bladder-cancer/statistics. Accessed September 2021.
10. NHS. Overview - Cystoscopy. https://www.nhs.uk/conditions/cystoscopy. Accessed September 2021.
11. Burger M et al. Eur Urol 2013; 64(5): 846–854.
12. Daneshmand S et al. Nat Rev Urol 2014; 11(10): 589–596.
13. Leal J et al. Eur Urol 2016; 69(3): 438–447.
14. Clark, O et al. Journal of Clinical Oncology Volume 41, Number 6; https://doi.org/10.1200/JCO.2023.41.6_suppl.479.